What is an Occupational Therapy SOAP Note?
In occupational therapy (OT), a SOAP note is a standardized medical record for documenting patient evaluation and treatment plans throughout therapy sessions. It stands for the four components required for this note: Subjective, Objective, Assessment, and Plan. Occupational therapists and assistants can use this note to keep track of a patient’s progress, evaluate the effectiveness of the implemented treatment plan, and adjust accordingly for optimal recovery.
Why is it Important?
SOAP notes are integral in occupational therapy for several reasons. At their core, they are vital for capturing patient information, such as their diagnosis and treatment plans. Therapists can leverage this data to monitor their patient’s progress, evaluate what is and isn’t working in the treatment plan, and make evidence-based judgments in adjusting their approach.
Moreover, they enable occupational therapists to communicate effectively with other healthcare professionals involved in a patient’s care. SOAP notes help ensure everyone has access to the same information about the patient’s treatment and progress. This ensures the continuity of quality care among healthcare providers.
What Should It Include?
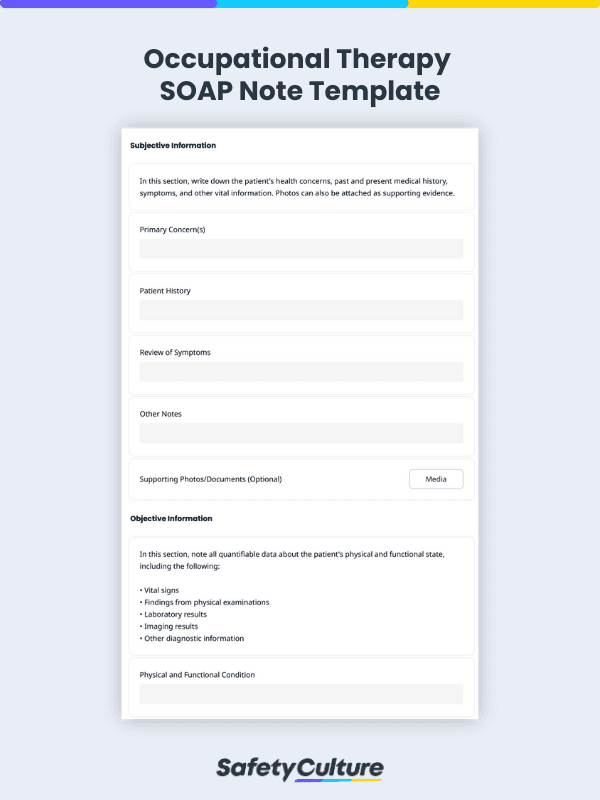
As mentioned earlier, an occupational therapy SOAP note should include the following sections:
Subjective
The first section of a SOAP note should contain information that the patient provides about their condition. It can include their primary concerns, symptoms, medical history, and other details that they feel are important to share.
When writing this section, it’s important to encourage the patient to be specific and descriptive about their symptoms. It also helps to use quotes from the patient to accurately encapsulate their concerns and feelings.
Objective
The next part of the SOAP note should collect objective data about the patient’s physical and functional abilities. In this section, be sure to include quantifiable metrics and health indicators such as the following:
Physical examination findings (e.g., range of motion, strength, coordination, balance)
- Vital signs
- Laboratory findings
- Imaging results
- Other diagnostic data
Assessment
The Assessment section of the SOAP note follows after gathering subjective and objective data from the patient. It’s dedicated to recording the occupational therapist’s professional opinion about the patient’s condition based on the information from the previous sections.
When writing this part, it’s best to be specific and transparent about the evaluation results and diagnosis. Moreover, for recovering patients, noting their progress and improvement areas can also help keep track of treatment goals.
Plan
The final section of the SOAP note is dedicated to the OT’s plan for treatment and goals for the patient’s progress. It should map out specific actions on the patient’s road to recovery, including the following information:
- Specific goals and objectives for the patient
- Interventions to achieve the goals (e.g., exercises, rehabilitation programs)
- Follow-up appointments (if any)
- Referrals to other healthcare providers (if applicable)
How to Write a SOAP Note in Occupational Therapy: Tips & Best Practices
After learning about the importance and components of an OT SOAP note, how can you write an effective one during therapy sessions? Here are 3 documentation practices to follow when drafting SOAP notes for occupational therapy:
Use Clear and Concise Language
OT SOAP notes should, first and foremost, be written clearly and concisely using simple language. As much as possible, avoid medical jargon and technical terms that other healthcare professionals may not be familiar with. This way, these providers and patients (if requested) can easily digest and understand the information provided.
Document SOAP Notes in a Timely Fashion
Timeliness is essential in OT SOAP note documentation, as it ensures that healthcare providers have up-to-date information readily available when making treatment decisions. Delays can also result in inaccuracies or incompleteness when logging data into the patient’s records.
Ideally, they should be entered into the patient’s medical record immediately after each session. However, if that’s not feasible, they should be encoded at the soonest time possible.
Ensure Accuracy and Completeness of Information
Aside from a timely completion, data accuracy and completeness are also vital for OT SOAP notes. These notes should contain complete and accurate information about the patient’s condition, progress, and treatment plan. Inaccurate records can have serious repercussions, from malpractice audits to reputational damage.
Thus, it’s best to avoid making assumptions or guesses about the patient’s condition without a solid basis. Instead, always refer to objective data and the patient’s self-reporting to ensure the veracity of information. Then, have these notes signed and dated by the OT practitioner as proof of completion.
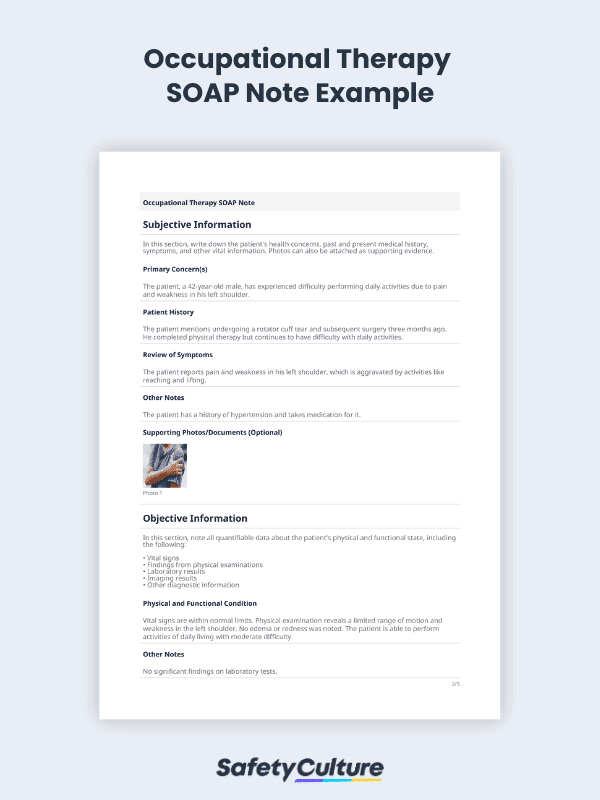
Occupational Therapy SOAP Note Example
To illustrate how this works, here’s an example of a SOAP note used in occupational therapy:
Subjective: The patient, a 42-year-old male, has experienced difficulty performing daily activities due to pain and weakness in his left shoulder. He reports pain and weakness in his left shoulder, which is aggravated by activities like reaching and lifting.
Objective: Vital signs are within normal limits. Physical examination reveals a limited range of motion and weakness in the left shoulder. No edema or redness was noted. The patient is able to perform activities of daily living with moderate difficulty.
Assessment: The patient is diagnosed with shoulder impingement syndrome secondary to a rotator cuff tear. His history of rotator cuff tear and surgery, as well as his symptoms and physical exam findings, support the diagnosis of shoulder impingement syndrome.
Plan: The patient will begin occupational therapy to improve his range of motion, strength, and functional ability in the left shoulder. Treatment will include therapeutic exercise, manual therapy, and education on joint protection techniques. The patient will also be advised to avoid aggravating activities and use pain management strategies as needed. Treatment progress will be monitored regularly, and adjustments made as necessary.
FAQs about Occupational Therapy SOAP Notes
SOAP notes in occupational therapy settings are typically written by licensed OT practitioners or by the assistants of OT practitioners. These help them monitor their patient’s progress over time and communicate effectively with other healthcare professionals to achieve continuity of care.
The frequency of creating SOAP notes in occupational therapy may vary depending on the patient’s condition and treatment plan. Some cases may warrant a new SOAP note for each session, while others may require periodic intervals (e.g., once a week or once a month).
In most instances, patients are entitled to access their medical records, including SOAP notes for occupational therapy sessions. To obtain these documents, they can submit a request to their OT practitioner or healthcare provider.